Long Covid Land Toolbox
A Case Definition of a New Disease: A Review of the US Working Definition (USG) and 2024 NASEM Definition for Long COVID

by Elisa Perego
Institute of Archaeology, University College London, 31-34 Gordon Sq, London WC1H 0PY, UK
Covid for Doctors - Dr Nancy Malek
The Long Covid Strategy Guide for Talking to Doctors


Notes for Friends – Articles on COVID-19
Substack by David
Your appointment was at 2:30. You’ve been sitting in this waiting room since 2:15, which means you’ve already burned through half your energy reserves for the day.
You’re clutching a carefully written list of symptoms that have plagued you since your Covid infection eight months ago. Brain fog that makes you feel like you’re thinking through molasses. Heart palpitations that wake you up at 3 AM. Fatigue so crushing that taking a shower feels like running a marathon.
You sit there counting ceiling tiles, trying not to cry.
You were early. You always are now. That’s the only way you can make it through the door, early, braced, list in hand, pretending you’re okay when you’re absolutely not.
You’ve rehearsed this visit like a courtroom deposition. Because that’s essentially what it’s become.
Long COVID: a clinical update
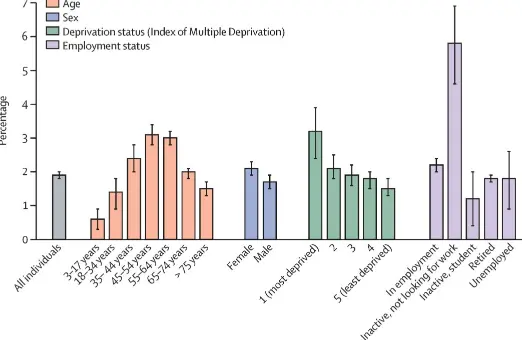
Post-COVID-19 condition (also known as long COVID) is generally defined as symptoms persisting for 3 months or more after acute COVID-19. Long COVID can affect multiple organ systems and lead to severe and protracted impairment of function as a result of organ damage. The burden of this disease, both on the individual and on health systems and national economies, is high. In this interdisciplinary Review, with a coauthor with lived experience of severe long COVID, we sought to bring together multiple streams of literature on the epidemiology, pathophysiology (including the hypothesised mechanisms of organ damage), lived experience and clinical manifestations, and clinical investigation and management of long COVID. Although current approaches to long COVID care are largely symptomatic and supportive, recent advances in clinical phenotyping, deep molecular profiling, and biomarker identification might herald a more mechanism-informed and personally tailored approach to clinical care. We also cover the organisation of services for long COVID, approaches to preventing long COVID, and suggestions for future research.

Perioperative and anesthetic considerations for
post-acute sequelae of COVID (PASC)/long COVID
Published:
Post-acute sequelae of COVID (PASC), commonly known as long COVID, presents with a broad spectrum of medical conditions and symptoms persisting beyond 3 months post-SARS-CoV-2 infection, affecting over 18 million Americans and 65 million people worldwide. Despite its prevalence, to date, there are no specific clinical guidelines for the perioperative management of PASC patients. PASC is a complex, multisystemic condition leading to neurological, respiratory, and endocrine sequelae, potentially resulting from persistent viral presence, immune dysregulation, and/or end-organ damage. This manuscript discusses the implications of these sequelae on anesthesia practice, emphasizing the need for vigilance in pre-operative assessments to identify PASC and associated conditions through detailed patient history, understanding of off-label medication use, and familiarity with medical terminologies like POTS, MCAS, and brain fog. Key perioperative considerations include cautious use of anesthetics, especially in patients with neurological and cardiovascular complications. Pulmonary management strategies for PASC patients, such as lung-protective ventilation and non-invasive post-operative support, could mitigate any perioperative respiratory complications. Finally, we underscore the importance of a multidisciplinary approach to manage PASC patients effectively during surgery, advocating for personalized anesthetic plans and calling for more evidence-driven guidelines for this emerging patient group as research progresses.

Review of organ damage from COVID and Long COVID:
a disease with a spectrum of pathology

2024 Jul 2;5(1):66–75. doi: 10.1515/mr-2024-0030
Long COVID, as currently defined by the World Health Organization (WHO) and other authorities, is a symptomatic condition that has been shown to affect an estimated 10 %–30 % of non-hospitalized patients after one infection. However, COVID-19 can also cause organ damage in individuals without symptoms, who would not fall under the current definition of Long COVID. This organ damage, whether symptomatic or not, can lead to various health impacts such as heart attacks and strokes. Given these observations, it is necessary to either expand the definition of Long COVID to include organ damage or recognize COVID-19-induced organ damage as a distinct condition affecting many symptomatic and asymptomatic individuals after COVID-19 infections. It is important to consider that many known adverse health outcomes, including heart conditions and cancers, can be asymptomatic until harm thresholds are reached. Many more medical conditions can be identified by testing than those that are recognized through reported symptoms. It is therefore important to similarly recognize that while Long COVID symptoms are associated with organ damage, there are many individuals that have organ damage without displaying recognized symptoms and to include this harm in the characterization of COVID-19 and in the monitoring of individuals after COVID-19 infections.

Cognitive impairment 2 years after mild to severe SARS-CoV-2 infection in a population-based study with matched-comparison groups

COVID-19 no longer constitutes a public health emergency of international concern1. However, a significant proportion of the population was exposed to COVID-19 in the first year of the pandemic. In this period, individual and group immunities to the disease were low and SARS-CoV-2 infection caused severe disease more frequently2.
Previous studies have reported higher risks of neurodegenerative diseases following the acute phase of SARS-CoV-2 infection compared to SARS-CoV-2-uninfected individuals3. These risks were even higher in the most severe cases of COVID-19 and in unvaccinated individuals4. Conversely, deficits in cognitive tests were reported to be higher in individuals with COVID-19 post-acute sequelae persistent for more than 12 weeks than in SARS-CoV-2-uninfected individuals…
